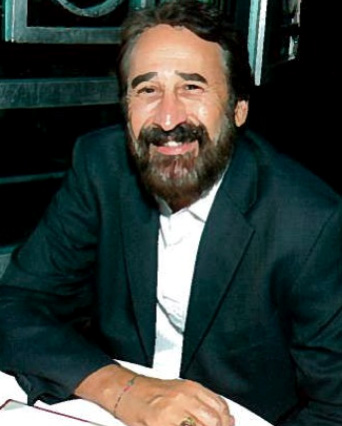
Professor and Vice Chair, and Chief of Psychiatry, University Hospital, Keck School of Medicine, University of Southern California
Care For Your Mind: As the provisions of the Affordable Care Act are implemented, what are the big changes you see for mental health care?
David Baron: Mostly, they are positive changes. More people will receive services whether under expanded Medicaid or purchasing insurance: this will enable them to seek care that they might not have had previously. The key will be making sure there are enough professionals to provide the care that people need and, of course, helping people to understand what kind of care they are entitled to.
CFYM: Which of those is the bigger challenge?
DB: It’s difficult to say. Access to a mental health professional is very challenging for anyone who lives more than fifty miles outside of a large urban area. Even in urban areas, there are nowhere near enough child psychiatrists, so it’s important to be able to rely on psychologists and social workers. This is where the concept of the “Medical Home” can be very valuable to mental health patients. We can try to fill those gaps and allow everyone involved in the care of the individual to work together to integrate mental health into the overall picture of the patient’s care.
Of course, the execution is important: this is a concept that we’re not entirely used to. Remember mental health has always been separate—there was even a time when the psychiatric hospital would be separated from the rest of the hospital buildings—so it’s important that we embrace these changes and make them work for patients.
We tried a somewhat similar experiment at Temple University in Philadelphia when I was there: we linked trained behavioral health specialists directly to the primary care provider’s office. It was very successful and the patients loved it, but after a while the health plan that we were working with on the program was bought by another carrier and the project was discontinued.
One of the unheralded benefits of an integrated care model is that it helps to reduce social stigma: many people are afraid to go to a mental health office. They have a fear that they will be seen going into the building, or that they will be sitting next to a potentially volatile person in the waiting room. This stigma prevents a lot of people from seeking care that they need.
CFYM: How do you overcome the barriers of fear and social stigma associated with mental illness?
DB: There’s no magic answer: in some cases, the stigma is a generational thing that is changing, but for many others, especially in some ethnic communities, there’s still a huge fear of mental illness. This is why public mental health literacy is so important.
We focus a lot on public health in other areas, educating people about vaccinations and neonatal care for instance, but as a country, we really need to work on educating people about mental illness. Not just to reduce the stigma, but also so that people and others who interact with them start to recognize symptoms and can seek help. If people were better educated on the early symptoms of a mood disorder, they would have a tool to understand what is happening if they start to feel a general sense of hopelessness or an inability to enjoy anything, and they would know to seek help.
It’s equally important for the people around them to recognize these symptoms for what they are and be able to speak up. We did a program in Italy to intervene in the high levels of adolescent suicide and depression. We targeted teachers, youth sports coaches, and anyone who would have regular contact with youths so that they would be aware of mood disorder symptoms.
CFYM: Tell us about the Tele-Health/Tele-Psychiatry program you are involved with to address access issues?
DB: This is a great program that harnesses all of the advances in technology of the past few years and enables us to reach out to a lot of patients who don’t live anywhere near a major mental health care facility. Many areas of medicine require hands-on contact between the patient and the physician, but psychiatry doesn’t necessarily need that for every patient. We can still have real-time human interaction with patients using phone and video.
Communication using phone and computer has become the norm for so many people, especially the younger generation, that it fits right in with their lifestyle. We’re doing cognitive behavior therapy using communications technology with patients and many of them are more comfortable with online and/or tele-psychiatry than with an in-person office visit. State government payors took the lead early on in this; private payors have lagged a little behind but they’re starting to embrace it. I think we can show that it can be a really cost-effective form of intervention.
Twenty-five years ago, we tried this in West Virginia and our first grant was $100,000. Now we can do the same thing for less than $1,000 and the quality of the video and connectivity are so much better. There are some issues that still have to be worked out (medical malpractice nuances, etc.), but we expect that this will be a meaningful way to reach people who have no local access to services.
CFYM: You work in a dense urban setting in downtown Los Angeles. Are there specific access challenges associated with that environment?
DB: Our biggest issue is dealing with the sizable population that have mood disorders but also alcohol and drug addiction issues. The Department of Mental Health is overwhelmed by the way it is currently handled. Typically patients are just dropped off at emergency rooms by police. Once they are sober, they are back on the streets within 24 hours without any intervention for the underlying problem—then back in the medical center again within a few days. We have to find a more clinically-effective and cost-effective way to manage patients with addiction and underlying mental health issues. We should at least be looking at how we can treat these patients through urgent care centers and relieve the pressure from ERs so that they get the immediate care they need but also so that they can be funneled to the longer-term care they also need.
CFYM: You’re very optimistic about the possibilities offered by newer models of health care. How can patients play a role in making these possibilities a reality?
DB: This is very, very important. We have to make sure that mental health becomes a critical part of how we are changing health care in this country. The demand cannot just come from psychiatrists: we see what’s needed, but we could be said to have a vested interest in expanding mental health care coverage and access. It’s critical for the patients and their families to speak up and demand that services are available. They have to go beyond complaining about the inadequacy of the current system and really be active advocates for change. The community can
- educate on the associated cost to society of untreated mental health disorders
- demonstrate how new treatment models can reduce health care expenses in a meaningful way
- insist that mental health care issues stay on the front burner
Politicians need to understand that mood disorders are treatable. We should all be working together to ensure that mental health is out in the open and is properly addressed. Right now we are at a generational transition in terms of how mental health is perceived, and we’re also at the right point in time policy-wise to demand changes and ensure they are a real part of the new model.









Connect With Us